We believe that every child matters and that the fundamental purpose of education is to prepare students to lead fulfilled, productive, responsible, happy and successful adult lives.
No items found.
We believe that every child matters and that the fundamental purpose of education is to prepare students to lead fulfilled, productive, responsible, happy and successful adult lives.
At Lift Crescent View, we believe in the importance of every child achieving their ‘best’, making good progress and enjoying their learning experience through 'High Quality Teaching'. As a school, when we plan any learning opportunity, our children and their needs are the central focus.
All of our children have provisions outlined in their EHCPs to meet their complex needs, there are also occasions when additional support is required to allow us to support the next steps in their learning journey. Additional support may be given for a set period of time or for a longer period to ensure every child can access our curriculum effectively and are fully included in learning opportunities and school events. Our parents/carers are informed, included and supported throughout such periods of provision.
At Lift Crescent View, teaching and learning opportunities are adapted and continually evaluated (with the support of external agencies when required) to ensure the needs of all of our children are met. Parents/carers should not feel unduly anxious about such additional support, which at our academy allows all children to receive the specific help they need to make the next steps in their exciting learning journey.
The Local Offer is a central source of information on services for children and young people aged 0-25 years with Special Educational Needs and Disabilities (SEND) and their families in Gloucestershire. It includes specialist activities and support.
The Government provides some advice for parents and carers about Special Educational Needs and Disabilities which you can access here https://www.gov.uk/children-with-special-educational-needs
View our SEND policies here
All our pupils have EHCPs plans, which are an integral part of our Assess, Plan, Do, Review cycle (more detail below).For details of the assessments, interventions and resources we use, please see Lift Crescent View Graduated Response document and the Interventions page.
Lift Crescent View uses a Graduated Response to needs which are first identified by assessment.
- Universal - Whole school assessment cycle including standardised summative assessment and teacher assessment. Effective inclusion of all pupils in daily, adapted and scaffolded high-quality lessons.
- Targeted - Small group or 1:1 assessment to identify needs leading to small group, time limited intervention to accelerate progress and to enable pupils to work at age-related expectations.
- Specialist - 1:1 individualised and targeted. For pupils who have complex needs or who are working well below age-related expectations. Likely to be life-long SEND needs. Assessment at this level will be with specialists.
For each area of need we have assessments and interventions for each level of response. The four areas of need are:
- Cognition and Learning (C&L) - including: Moderate learning difficulties (MLD); Severe learning difficulties (SLD); Specific learning difficulties (SpLD), for example Dyslexia, Dysgraphia, Dyspraxia (DCD) and Dyscalculia; Executive Functioning Differences; etc.
- Communication and Interaction (C&I) - including: Speech, language and communication needs (SLCN); Specific learning difficulties (SpLD); Autism (ASD); Hearing impairment (HI); etc.
- Social, Emotional & Mental Health (SEMH) - including: Attention deficit disorder (ADD); Attention deficit hyperactivity disorder (ADHD); Obsessive compulsive disorder (OCD); Oppositional defiance disorder (ODD); Autism (ASD); Bipolar disorder; Anxiety disorder, etc.
- Physical and Sensory (P&S) - including: Visually impaired (VI); Hearing impaired (HI); Multi-sensory impaired (MSI); Physical disability (PD); Sensory processing differences (SPD); Dyspraxia (DCD), etc.
We welcome students with special educational needs or disabilities and support students across four teams. Students are organised into the teams during their transition from their previous school and it is based on the student’s main area of need. An Area of Need leader will monitor their academic progress and attendance whilst ensuring that the student’s needs were been met both through teaching and structured interventions.
For students with specific learning difficulties such as dyslexia, or moderate learning difficulties that affect students in a range of cognitive areas.
For students who struggle to engage in the social aspects of school, or who find it hard to cope with challenging emotions. This will range from students needing short-term assistance during a turbulent time in their life, to students with a recognised condition such as ADD or ADHD.
For students who have speech, language and communication needs, a specific language impairment or a range of communication difficulties. Students who find it difficult to interact with others are supported within this area.
Students whose need is primarily sensory and, or physical have their support overseen by the area of need leader in this team. This team would support students with hearing or visual impairments as well as students with physical needs.
Initial visits to Lift Crescent View are welcomed on Friday afternoons 1:30-3:00pm, please contact the school office to arrange on 01242 512 680 or email us at contactus@liftscrescentview.org
Prospective Parents/Carers
Welcome to Lift Crescent View
Please see our welcome pack here:
All admissions are agreed through consultation by the Local Authority (LA)
Process of admission:
Children and young people with special educational needs may get help with travel to school or college, but it is not an automatic right. An assessment is made of the child's needs and individual circumstances with all decisions made and managed by the Gloucestershire Local Authority.
A door-to-door service is provided only in specific circumstances. Children may have to travel to their nearest pickup point.
To see if you're eligible please fill in an assessment form that you can find by following this link, paper copies are available from the school office.

At Lift Crescent View we have 2 layers of assessments:
The further assessments include specific assessments for: sensorimotor development; speech, language and communication needs (SLCN); specific learning difficulties (SpLD); phonological processing; and visual stress. We will always inform you and ask for consent when a further assessment is being completed for your child and the results from this shared.
When we have assessed to understand the specific areas of need the class teacher in liaison with the SENDCo will design an intervention plan to meet the need and close the gaps in the pupil’s understanding.
l our pupils have an EHCP which are managed by the Local Authority (LA), however the the LA defer many management activities to the school. The SEND CoP (Special Educational Needs & Disability Code of Practice, 2014) lays out in law that all EHCPs must be reviewed annually.
The school plans their annual reviews by year group, following this pattern:
A pupil may require an early or emergency review, this will always be in discussion with the child's parents/carers and the LA.
Every pupil also has a My Plan which is developed from the outcomes identified on the EHCP, breaking down them down into managable small steps and SMART targets.
SMART targets should be Specific Measurable Achievable Relevant and Time-bound
Pupils are invited to work with teaching staff to review and rewrite targets and provisions and pupils' views are collected freshly for each plan written. Pupils have their targets displayed in the classroom, either on an accessable display board or on their desks and are encouraged to add stickers when they feel they have met their targets. This allows them to have ownership over their targets and drives progress forward.
Parents will be asked to take part in the reviewing and production of plans during parents evenings which occur 3 times a year. The dates for the My Plan cycle at Lift Crescent View are: October half-term, February half-term and May half term, we then do a mini review in July, ready for the new academic year.
Where pupils are Children Looked After and have Personal Education Plans (PEPs) these will be written to link to the My Plans to ensure clarity of offer.
Class staff are supported by the Intervention Team and the Senior Leadership Team, to use a range of strategies, approaches and evidence based interventions, based on the individual pupil’s gaps in learning. Where possible we try and embed the provisions into normal classroom practice so that skills are generalised and not learned for a specific environment.
Take a look at the Lift Crescent View Graduated Response for details of interventions we access.
In lessons we teach the National Curriculum for the year group, using a combination of bought schemes and schemes from our Trust (Lift Schools). We then adapt the way in which we present, support and scaffold the learning to meet the individual needs of the pupils. Please see the Curriculum pages for details of what we teach.
Interventions planned by specialist professionals, for example Educational Psychologist, Speech and Language Therapist and Occupational Therapist, will be run by the class staff and the Intervention Team.
Review of targets happens through a combination of marking and assessment:
Once the assessment has been completed the plan can be reviewed and rewritten with the pupil and parents on the schedule seen in the Plan section.
In educational settings, interventions are often used to describe a focused teaching session, which is a deviation away from existing teaching practice. Interventions in schools can be one-to-one, or delivered as a group.
At Lift Crescent View we use a number of different interventions to meet the variety of needs our pupils have, here are just a few. If you would like to know about all of them see our Graduated Response document.
Intervention Team
The Lift Crescent View Intervention Team work with children from across the school using a range of planned and ad hoc interventions that meet and adapt to the needs of the children. They support the SaLT and OT by carrying out screening activities and support with daily interventions. They are ace bakers and crafty crafters to support the children in making and creating alongside talking about their emotions and reactions.
The team are all trained by the Trauma Action Group as practitioners and in meeting children's SEMH needs.
Laura Brown, Speech & Language Therapist (SaLT)
Laura is an experienced Speech and Language Therapist having worked with children for over 20 years. Laura understands the importance of making sessions fun and engaging for children and always seeks to understand their interests in order to incorporate them into sessions.
Laura supports the school one day a week to screen, assess and design intervention plans supporting the class and intervention staff to deliver the support each individual pupil needs. Laura also supports teaching staff to match the language in the classroom to the pupil's understanding.
Lift Crescent View screens all pupils each year for higher level language skills and Blanks levels, which Laura uses to advise classroom staff on the use of language in the class to make it as inclusive as possible.

Elen Lloyd, Occupational Therapy (OT)
Elen supports the school one day a week, screening and assessing the children and supporting with developing and embeding intervention in the classroom. Watch her introduction video for more information.
The Trauma Action Group's mission is 'to improve as many people's lives as we can through better recognising and reducing the impact of psychological trauma.'
TAG are supporting us to become a Trauma Action Organisation by delivering training to all staff to understand the impact of trauma, how to support children in trauma and how to intervene and improve children's social-emotional understanding and skills.
A Trauma Action Organisation understands and responds to trauma in constructive and compassionate ways. Staff understand the role they play in reducing the prevalence of trauma and engage with the people they support to deliver better outcomes. Leaders create positive environments and role-model the right behaviours, helping eliminate practices which might cause or trigger trauma.

Language for Thinking is a structured approach to develop children’s language from the ‘here and now’ to the ‘how and why’. 50 colour drawings form the backbone of the resource. Written scenarios and question sheets are provided so adults can ask carefully promote children’s verbal reasoning and thinking skills.
At Lift Crescent View we assess all pupils for Language for Thinking levels to inform the use of language within the classroom. Language for Thinking levels are based around Blank levels of language (Blank, Rose & Berlin, 1978), see this video for information .
The dialogue between teacher and student that underpins learning frequently involves students being asked questions. However, a significant proportion of children find it difficult to understand these increasingly complex questions, including those with autism, social communication disorder, Developmental Language Disorder and learning difficulties. They may be able to understand simple and direct language, but when required to ‘read between the lines’ they struggle. This difficulty with questions may an impact on their understanding of social situations as well as reading comprehension.
Language for Behaviour and Emotions is a practical, interactive resource is designed to be used by professionals who work with children and young people who have Social, Emotional and Mental Health needs and Speech, Language and Communication needs.
Gaps in language and emotional skills can have a negative impact on behaviour as well as mental health and self- esteem. Language for Behaviour and Emotions provides a systematic approach to developing these skills so that young people can understand and work through social interaction difficulties.
A sensory circuit is a form of sensory integration intervention. It involves a sequence of physical activities that are designed to alert, organise and calm the child. The sensory circuit aims to facilitate sensory processing to help children regulate and organise their senses in order to achieve the ‘just right’ or optimum level of alertness required for effective learning. The circuit should be an active, physical and fun activity that children enjoy doing.
Sensory Integration is the process by which the brain receives, organises and processes all the information received from the senses. The senses include touch, sight, hearing, smell, taste, body position and movement (proprioception) and balance/position against gravity (vestibular). The information received from these senses help us to make sense of the world. Effective sensory integration and processing enables us to respond appropriately to different stimuli in our environment and informs our everyday functioning.
An inability to effectively process, organise and correctly interpret sensory information is known as Sensory Processing Disorder (SPD), formally known as sensory integration dysfunction. Children with SPD may find functional daily activities challenging. The severity of these difficulties can vary greatly. However, 1 in 6 children experience significant disruption to their daily lives as a result of SPD. When screened the large majority of our pupils have sensory integration differences.

We all have mental health, and like physical health, it can fluctuate depending on our circumstances and experiences. The World Health Organization defines emotional and mental health as “a state of well-being in which every individual realises his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to contribute to their community.”
When we refer to children and young people having emotional and mental health needs, we are typically talking about those who may feel overwhelmed by life’s challenges, who may struggle to find joy in everyday experiences, or who find it difficult to reach their full potential in learning and development.
The SEN Code of Practice (2015) broadens this definition by including the word ‘social’, recognising that emotional and mental health is often closely linked with a young person's social experiences. These needs may be influenced by relationships within their family, peer group, and wider community. In some cases, children may also experience barriers that make social interaction itself difficult, further impacting their overall well-being.

SEMH needs can sometimes arise from unmet or complex neurodevelopmental needs, for example: attention deficit hyperactivity disorder (ADHD); Tourette’s syndrome; and Autism.
SEMH needs can sometimes arise from a child or young person’s experiences and how these have been responded to and supported by others. Some children may have experienced adverse childhood experiences (ACEs) which, depending on support systems and prevalence, can increase stress and stress responses. There are other experiences such as bereavement, loss, health needs and traumatic events which can impact on wellbeing and these can be ongoing for several years after a particular event. For many children their prior educational experiences have led to trauma as the environment or challenges of the mainstream school have negatively affected them.
When children and young people persistently behave in a challenging way this is often a way of communicating that something is wrong. It is a sign that they are dysregulated or in distress.
Some children and young people get stuck in patterns of challenging behaviour and struggle to develop strategies they can use to feel calmer. It can be difficult for a child or young person to change their coping strategies when the circumstances and needs behind their behaviours remain the same.
Children and young people need to have coping behaviours modelled and supported by empathetic and attuned or ‘emotionally available’ adults.
At Lift Crescent View, we view every child as an individual with their own unique set of needs. Social, Emotional and Mental Health (SEMH) difficulties never stem from a single cause, and we are committed to interpreting each child’s behaviour as a form of communication—an insight into their unmet needs.
We adopt a relational approach that prioritises getting to know each pupil deeply—their strengths, interests, and the barriers they face. Relationships are at the heart of everything we do, and our success as a school is rooted in the strength of these connections.
All staff at Lift Crescent View receive extensive training to understand and respond to the impact of trauma. This may arise from a pupil’s home environment, from previous school experiences where their needs were unmet, or from the overwhelming nature of sensory or social environments. Our training includes Trauma-Informed Practice, Emotion Coaching, Restorative Approaches, Sensory Processing Differences, Speech, Language and Communication Needs (SLCN), Autism, ADHD, and a wide range of evidence-based strategies that enable us to create inclusive and responsive classrooms where pupils can thrive.
Social and emotional development is embedded across the school day and curriculum. Each term, we introduce a whole-school book that is shared in class and assemblies, led by the Principal. Weekly challenges are then set for pupils that explore key themes from the book, encouraging emotional growth and social connection. Examples include:
Through a consistent, boundaried, and relational approach, we use play, curiosity, and positive relationships—our most powerful tool—to meet our pupils where they are. In doing so, we create a safe, nurturing space where they can succeed both emotionally and academically.
Trauma-Informed Practice
Trauma-informed practice is an educational approach based on the understanding that exposure to trauma can significantly affect a person's neurological, biological, psychological, and social development.
This approach seeks to raise awareness of how trauma may negatively influence a child’s ability to feel safe, regulate emotions, and build trusting relationships—both within the school setting and in wider social contexts. It recognises that behaviours often stem from unmet needs or past experiences, rather than intentional defiance or disruption.
At its core, trauma-informed practice aims to create a safe, inclusive, and culturally sensitive school environment—one that children, families, and communities feel they can trust and where they feel valued. It emphasises the importance of consistency, compassion, and connection in building the foundations for learning and emotional development.
This approach equips school staff to work in genuine collaboration with children and their families, promoting shared decision-making and empowering individuals to take ownership of their health, wellbeing, and educational journey.
Rather than asking, “What is wrong with this person?”, trauma-informed practice invites us to ask, “What has happened to this person, and what do they need?”. It shifts the focus from behaviour management to understanding and support, enabling us to respond to pupils with empathy, patience, and skill.

Neurosequential Model
The Neurosequential Model is a developmentally-informed and biologically-respectful approach that helps educators understand how brain development and early life adversity impact a child’s behaviour, emotional regulation, and capacity to learn. Developed by Dr. Bruce Perry, the model highlights the critical importance of aligning educational and therapeutic interventions with the specific areas of the brain affected by trauma and developmental disruption.
In classroom settings, the Neurosequential Model provides a framework to better support children who have experienced developmental trauma. Central to this approach are the three R’s:
This sequence is vital. A dysregulated brain cannot engage in relationships or higher-order thinking. Learning, reasoning, and behaviour change are only possible once a child feels physically and emotionally safe.
At The Ridge Academy, we embed the principles of the Neurosequential Model in our daily practice. By prioritising regulation and connection before expectation, we create the conditions necessary for children to thrive academically, socially, and emotionally.
Emotion Coaching
Emotion Coaching, defined by Gottman, 1997, is based on the principle that nurturing and emotionally supportive relationships provide optimal contexts for the promotion of children's outcomes and resilience.
Emotion Coaching uses moments of heightened emotion and resulting behaviour to guide and teach the child and young person about more effective responses. Through empathetic engagement, the child's emotional state is verbally acknowledged and validated, promoting a sense of security and feeling 'felt'. This activates changes in the child's neurological system and allows the child to calm down, physiologically and psychologically.
Restorative Approach
Restorative Approach is value–based and needs–led. Restorative Practice is a 'way of being' where the focus is on building strong, meaningful, trusting and respectful 'relationships', and repairing relationships when difficulties or harm arises. This leads to a cohesive community as the foundations on which good teaching and learning can flourish. In such a community young people are given a lot of responsibility for decision-making on issues that affect their lives, their learning and their experience of school. Restorative Approaches build upon the basic principles and values of humanistic psychology:
PACE approach, PACE stands for Playfulness, Acceptance, Curiosity and Empathy.
PACE is a way of thinking, feeling, communicating and behaving that aims to make children feel safe. It is particularly effective in meeting the needs of children who have experienced trauma. Developed by clinical psychologist, Dan Hughes, the approach focuses on building trusting relationships, emotional connections, containment and a sense of security.
The principles offer a useful framework from which we can develop attunement and strengthen our relationships with the children and young people we work with.
Playfulness:
Acceptance:
Curiosity:
Empathy:
Autism is a lifelong developmental disability which affects how people communicate and interact with the world. More than one in 100 people are on the autism spectrum and there are around 700,000 autistic adults and children in the UK. Autism is a spectrum condition and affects people in different ways. Like all people, autistic people have their own strengths and weaknesses. Below is a list of difficulties autistic people may share, including the two key difficulties required for a diagnosis. (from NAS website www.autism.org.uk, April 2024)
Social communication and social interaction challenges
Social communication
Autistic people have difficulties with interpreting both verbal and non-verbal language like gestures or tone of voice. Some autistic people are unable to speak or have limited speech while other autistic people have very good language skills but struggle to understand sarcasm or tone of voice. Other challenges include:
Social interaction
Autistic people often have difficulty 'reading' other people - recognising or understanding others' feelings and intentions - and expressing their own emotions. This can make it very hard to navigate the social world. Autistic people may:
Repetitive and restrictive behaviour
With its unwritten rules, the world can seem a very unpredictable and confusing place to autistic people. This is why they often prefer to have routines so that they know what is going to happen. They may want to travel the same way to and from school or work, wear the same clothes or eat exactly the same food for breakfast.
Autistic people may also repeat movements such as hand flapping, rocking or the repetitive use of an object such as twirling a pen or opening and closing a door. Autistic people often engage in these behaviours to help calm themselves when they are stressed or anxious, but many autistic people do it because they find it enjoyable.
Change to routine can also be very distressing for autistic people and make them very anxious. It could be having to adjust to big events like Christmas or changing schools, facing uncertainty at work, or something simpler like a bus detour that can trigger their anxiety.
Over- or under-sensitivity to sensory information
Autistic people may experience over- or under-sensitivity to sounds, touch, tastes, smells, light, colours, temperatures or pain. For example, they may find certain background sounds like music in a restaurant, which other people ignore or block out, unbearably loud or distracting. This can cause anxiety or even physical pain. Many autistic people prefer not to hug due to discomfort, which can be misinterpreted as being cold and aloof.
Many autistic people avoid everyday situations because of their sensitivity issues. Schools, workplaces and shopping centres can be particularly overwhelming and cause sensory overload. There are many simple adjustments that can be made to make environments more autism-friendly.
Highly focused interests or hobbies
Many autistic people have intense and highly focused interests, often from a fairly young age. These can change over time or be lifelong. Autistic people can become experts in their special interests and often like to share their knowledge. A stereotypical example is trains but that is one of many. Greta Thunberg's intense interest, for example, is protecting the environment.
Like all people, autistic people gain huge amounts of pleasure from pursuing their interests and see them as fundamental to their wellbeing and happiness.
Being highly focused helps many autistic people do well academically and in the workplace but they can also become so engrossed in particular topics or activities that they neglect other aspects of their lives.

Extreme anxiety
Anxiety is a real difficulty for many autistic adults, particularly in social situations or when facing change. It can affect a person psychologically and physically and impact quality of life for autistic people and their families.
It is very important that autistic people learn to recognise their triggers and find coping mechanisms to help reduce their anxiety. However, many autistic people have difficulty recognising and regulating their emotions. Over one third of autistic people have serious mental health issues and too many autistic people are being failed by mental health services.
Meltdowns and shutdowns
When everything becomes too much for an autistic person, they can go into meltdown or shutdown. These are very intense and exhausting experiences.
A meltdown happens when someone becomes completely overwhelmed by their current situation and temporarily loses behavioural control. This loss of control can be verbal (eg shouting, screaming, crying) or physical (eg kicking, lashing out, biting) or both. Meltdowns in children are often mistaken for temper tantrums and parents and their autistic children often experience hurtful comments and judgmental stares from less understanding members of the public.
A shutdown appears less intense to the outside world but can be equally debilitating. Shutdowns are also a response to being overwhelmed, but may appear more passive - eg an autistic person going quiet or 'switching off'. One autistic woman described having a shutdown as: 'just as frustrating as a meltdown, because of not being able to figure out how to react how I want to, or not being able to react at all; there isn’t any ‘figuring out’ because the mind feels like it is past a state of being able to interpret.'
At Lift Crescent View we look at each child very much as an individual with individual needs. Autism doesn't fall into one singular profile, we use our experience and training to interpret a child's behaviour as communication of their underlying needs. We use routines and boundaries to guide pupils through their day, rewards are regular and often and consequences are agreed through Restorative Practices.
All of our staff have training in Trauma Informed practices, Emotion coaching, Restorative practices, Sensory processing differences, Speech, Language and Communication Needs, Autism, ADHD, etc. and many other specific tools and strategies that allow us to create classrooms and approaches for our pupils to thrive.
Through our consistant boundaried approach we use fun and our most important tool our relationships to support our pupils with their needs allowing them to succeed in a safe space.
We use the following practices to support our children:
Routines, Boundaries and Structure:
“Reality to an autistic person is a confusing, interacting mass of events, people, places, sounds and sights... Set routines, times, particular routes and rituals all help to get order into an unbearably chaotic life. Trying to keep everything the same reduces some of the terrible fear.” Jolliffe (1992) in Howlin (2004), p.137.
The world can seem a very unpredictable and confusing place to autistic people, who often prefer to have a daily routine so that they know what is going to happen every day. They may want to always travel the same way to and from school, or eat exactly the same food for breakfast. Rules can be very important for some autistic people. It may be difficult for an autistic person to take a different approach to something once they have been taught the 'right' way to do it.
Sometimes minor changes such as moving between two activities, can be distressing; for others big events like holidays, starting or changing school, moving house or Christmas, which create change and upheaval, can cause anxiety.
Some autistic people have daily timetables so that they know what is going to happen, when. However, the need for routine and sameness can extend beyond this. You might see:
People's dependence on routines can increase during times of change, stress or illness and may even become more dominant or elaborate at these times.
Unexpected changes are often most difficult to deal with. Autistic people may not be comfortable with the idea of change, but may be able to manage it better if they can prepare for changes in advance.
Visual supports
Visual supports are a communication tool that can be used with autistic people. They can be used in most situations, are adaptable and portable.
Visual supports can help to:
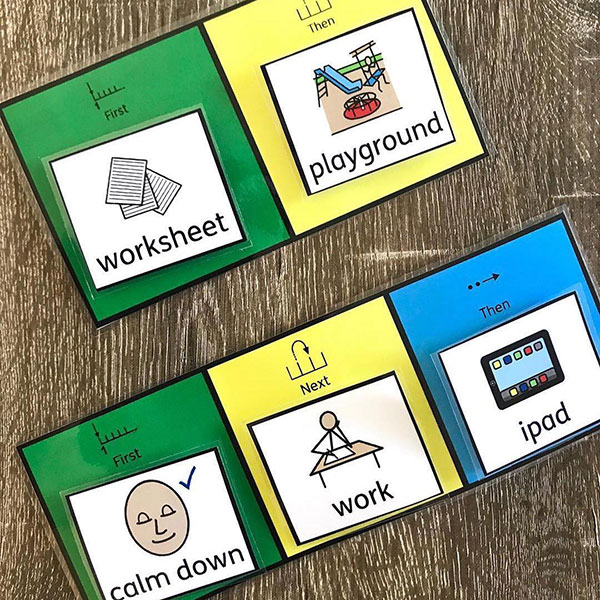
They can make communication physical and consistent, rather than fleeting and inconsistent like spoken words can be.
We use visual timetables in all the classes
Wherever possible we show the children photos of a new place (eg a new class, visit environment), person (eg a new support worker) or activity (eg swimming). Make a book of photos, or a collection of images on their device, so they can look at it before and during the change.
We use visual supports to show the outcome of certain activities. For example, if you are going on holiday, just showing them a picture of an aeroplane may make them reluctant and nervous to go on a plane - they may not see the relevance of the plane. Show pictures of the whole process instead, including your destination. This will help them to understand the whole situation better. Reverse the series of pictures to show the return journey.
On the day of the change a visual timetable can be useful to explain exactly what will be happening.
Understanding ADHD
ADHD is a neurodevelopmental condition and NOT a behavioural disorder. That means the brain grows and function in different ways. ADHD is very common and occurs in approximately 1 in 20 people. ADHD can be especially challenging when you are young but can become easier for many when their brain reaches full maturity in their early 20s.
In adulthood, many people learn to use their self-knowledge to develop jobs and careers that play to their strengths and/or have developed strategies to support their needs.
ADHD can feel different for different people, for some people it can include challenges with attention, either struggling to maintain attention, even when the topic is important, for others its about 'hyperfocus' focussing for long periods of time on only one topic to the exclusion of all others. Many struggle with both inattention and hyperfocus at different times of their day, week, life.
For some people they experience physical hyperactivity or impulsivity, others verbal hyperactivity or internal hyperactivity when thoughts race.
There is more known about ADHD every year and there is a lot of support out there to help us understand ADHD. Key sources of quality information can be found at:
At Lift Crescent View we look at each child very much as an individual with individual needs. ADHD doesn't fall into one singular profile, we use our experience and training to interpret a child's behaviour as communication of their underlying needs. We use routines and boundaries to guide pupils through their day, rewards are regular and often and consequences are agreed through Restorative Practices. We use sensory circuits, movement breaks and a range of resources to meet children's individual needs.
All of our staff have training in Trauma Informed practices, Emotion coaching, Restorative practices, Sensory processing differences, Speech, Language and Communication Needs, Autism, ADHD, etc. and many other specific tools and strategies that allow us to create classrooms and approaches for our pupils to thrive.
Through our consistant boundaries approach we use fun and our most important tool our relationships to support our pupils with their needs allowing them to succeed in a safe space.
We use the following practices to support our children:
Routines, Boundaries and Structure:
Structure means that the environment is organised and predictable. Structure is important for all children, but it can be particularly important if you are supporting a child with ADHD.
Having a routine can benefit a child with ADHD and the rest of the school. Structure is beneficial for several reasons:
When children have day-to-day routines and a schedule to follow, this creates structure in their lives. Consistent rules, expectations, and consequences clearly understood by the child (and positively reinforced by the adults) help maintain a predictable environment.
In a structured environment, children know what to expect. This knowledge creates a sense of security, so most children benefit from structure whether they have ADHD or not.
PACE approach, PACE stands for Playfulness, Acceptance, Curiosity and Empathy.
PACE is a way of thinking, feeling, communicating and behaving that aims to make children feel safe. It is particularly effective in meeting the needs of children who have experienced trauma. Developed by clinical psychologist, Dan Hughes, the approach focuses on building trusting relationships, emotional connections, containment and a sense of security.
The principles offer a useful framework from which we can develop attunement and strengthen our relationships with the children and young people we work with.
Playfulness:
Acceptance:
Curiosity:
Empathy:
ADHD, Autism, Learning Difficulties, and similar conditions are neurodevelopmental in nature—meaning their symptoms, behaviours, and traits arise from the way a person’s brain develops during critical stages of early development, either before birth or in early childhood.
Conditions are said to co-occur when they are found in the same person at the same time. This is different from co-morbidity, which implies that the conditions are unrelated. Neurodiverse conditions co-occur at very high rates. For example: Approximately 1 in 2 people with ADHD have dyslexia, Approximately 1 in 2 people with ADHD have dyspraxia, 9 in 10 people with Tourette's have ADHD, 2 in 3 people with ADHD have autistic spectrum traits, and people with ADHD are 8-fold more likely to meet full criteria for an autistic spectrum diagnosis (From 'Neurodevelopmental conditions' on ADHDaware.org.uk, as of May 2024)
Examples of Co-occurring conditions are: Sensory Processing Disorder (SPD), Tourettes, Anxiety, Obsessive Compulsive Disorder (OCD), Developmental Language Disorder (DLD)
A specific learning difficulty (SpLD) means that someone has a difference or difficulty with one or more certain parts of learning. Having a SpLD does not mean that children and young people cannot achieve and succeed in learning. Some examples of SpLD are: Dyslexia, Dyscalculia, Dysgraphia, Dyspraxia or Developmental Coordination Disorder (DCD). SpLDs are thought to affect at least 10% of the population.
SpLDs affect the way information is processed and learned, which can have a very significant impact on formal education and study, and subsequently often on self-confidence as well. However, SpLDs are neurological and are unrelated to intellectual ability, socio-economic or language background. Students with SpLD can have significant compensatory strengths in other areas of study and can be creative and innovative thinkers.
For details of the assessments, interventions and resources we use, please see The Ridge Graduated Response document
Sensory Processing Disorder (SPD) is a term used to describe children who struggle to correctly perceive the sensory world around them.
SPD can be present in many forms and can often result in behavioural issues as well as functional difficulties. It is common for children within the Autistic Spectrum to experience many complex sensory difficulties. Children with SPD may experience sensory difficulties relating to one or multiple senses. Some of the symptoms of SPD are: Poor posture; Difficulty controlling movements; Poor handwriting; Dislikes loud noises; Difficulty making friends; Difficulty dressing, eating or sleeping; Frequently throws tantrums or gets upset; Easily distracted; Fidgety
Examples of how we support SPD
1 out 15 people in the UK have a hidden but common condition (disability) called Developmental Language Disorder (DLD) and they feel invisible. That’s the equivalent of two children in the average classroom.
DLD is a diagnosis given by a speech and language therapist to people who have lifelong difficulties with talking and understanding words. These difficulties create barriers to communication or learning in everyday life and aren’t due to another condition.
Examples of how we support DLD
Dyslexia mainly affects literacy and language-related skills. It is characterised by weaknesses in the fluency and accuracy of reading and writing and in the speed and quantity of information which can be processed at any one time. There might also be difficulties with aspects of fluency, organisation of ideas and sequencing in reading, writing, and, in some cases, speaking.
Examples of how we support Dyslexia
Dysgraphia is a neurological condition that can affect written expression and fine motor skills. Not to be confused with similarly-sounding dyslexia, dysgraphia affects a person’s ability to organize and express thoughts and ideas in written form.
Writing is more than just putting pen to paper! Your brain needs to compute a complex set of instructions to process language in your mind, and then send those messages to your muscles in your hand and out onto the page, letter by letter.
Dysgraphia: from dys- ‘difficult’ + Greek -graphia ‘writing’.
Examples of how we support pupils with Dysgraphia:
Dyspraxia/Developmental Co-ordination Disorder (DCD) is characterised at its core by needs or underdevelopment in fine and/or gross motor co-ordination, but also by difficulties with organisation skills and sometimes visual perception. This can result in problems with writing by hand, concentration, personal and work organisation, time management and social difficulties.
Examples of how we support pupils with Dyspraxia/DCD:
Lift Crescent View,
Clyde Crescent,
Cheltenham,
GL52 5QH